Imagine waking up every day with an unrelenting ache in your lower back, a sharp stabbing pain in your joints, or a throbbing headache that won't go away. For billions of people worldwide, this is a reality they face daily. Pain is a complex and often debilitating condition that affects a significant portion of the population, impacting their daily lives and quality of life. Effective pain communication is crucial in facilitating proper pain management, as it allows healthcare providers to understand better the nature and intensity of a patient's pain. In this blog, we will delve into the world of pain, exploring the different types of pain, the importance of describing pain accurately, and the various treatment options available to those suffering from this condition. With this comprehensive overview, we aim to empower individuals to take control of their pain and improve their quality of life. To begin our journey into chronic pain, it is essential to understand the different types of pain and how they are measured.
What Types of Pain Are There?
Chronic pain is a complex and often debilitating condition that can take many forms. One way to categorize the different types of pain is by distinguishing between nociceptive, neuropathic, and psychogenic pain. Nociceptive pain is the most common type of chronic pain and is caused by the activation of pain receptors in response to tissue damage or injury. This pain is often associated with arthritis, back pain, or injury-related pain. Nociceptive pain is typically described as a throbbing, aching, or sharp pain and is usually responsive to pain medications. On the other hand, neuropathic pain is caused by damage or dysfunction within the nervous system and is often described as burning, tingling, or shooting pain. Nerve damage, spinal cord injuries, or certain neurological disorders can cause this pain. Neuropathic pain is often less responsive to traditional pain medications and may require a more specialized approach to management. Psychogenic pain, as the name suggests, is rooted in psychological factors and can be caused by stress, anxiety, or depression. This type of pain is often less defined and may be difficult to locate, making it challenging to diagnose and treat. Psychogenic pain is typically managed through a combination of psychological and medical interventions.
How Can You Identify Types of Pain?
Healthcare providers often use scales such as the numeric rating scale, Wong-Baker FACES pain rating scale, and visual analog scale to assess and measure pain accurately. These scales provide a standardized way of quantifying pain intensity and allow healthcare providers to track pain over time. Acute pain is a normal response to injury or tissue damage and typically subsides once the underlying issue has been resolved. Chronic pain, on the other hand, persists beyond the expected healing time and can significantly impact a person's daily life and quality of life.
How Can You Describe Pain?
As chronic pain sufferers know all too well, the experience of pain is highly subjective and can vary significantly from person to person. Therefore, to effectively communicate the nature of their pain, individuals must be able to describe it in detail.
-
Radiation and Localization: When it comes to pain, it's not just about the "ouch" factor in one spot; it's also about whether that "ouch" might spread to other areas. For example, pain that starts in your arm might spread to your rib. It's like a game of pain telephone, with the discomfort spreading from one place to another.
-
Interventions and Pain Tweaking: Understanding what makes the pain better or worse is crucial in figuring out the root cause and coming up with a plan to help. Pain might get louder when you lie down, take a deep breath, or touch the affected area. But it might also get quieter with the use of heat or ice, like turning down the volume on a radio. By understanding these modifications, healthcare providers can better handle the pain and create a treatment plan.
-
Intensity: To get a sense of the pain's severity, we often use a numerical scale, like a scale from one to 10. Checking in regularly on the pain intensity helps track its progression and see if treatments are working. It's like a scorecard for the pain, giving healthcare providers a sense of how the pain is changing over time.
-
Duration: The length of time that the pain lasts is also crucial in determining its cause and severity. This includes the pain's timeline and any patterns or fluctuations in how long it lasts. The duration of the pain can provide important information for healthcare providers in determining the best course of treatment.
-
Trigger: Knowing what set off the pain seems obvious but is no less important to keep front of mind. This could be a specific injury, activity, or a gradual onset over time. Keeping a pain journal is one of the most effective ways to help tell your pain story to healthcare professionals.
-
Recent History: The recent history of the person experiencing the pain is also important in getting the full picture. This includes changes in lifestyle, diet, overall health, and significant events or stressors that may have preceded the onset of pain. By taking the recent history into account, healthcare providers can better understand the person's overall health and how it might contribute to the pain.
-
Impact on Daily Activities and Quality of Life: The experience of chronic pain can have a profound impact on an individual's everyday life, affecting their ability to work, participate in leisure activities, and maintain relationships. How a person's pain impacts their daily activities and quality of life can be just as important as describing the pain itself. For example, is your pain impacting your ability to concentrate during work? No detail is too small.
How Can You Address Pain?
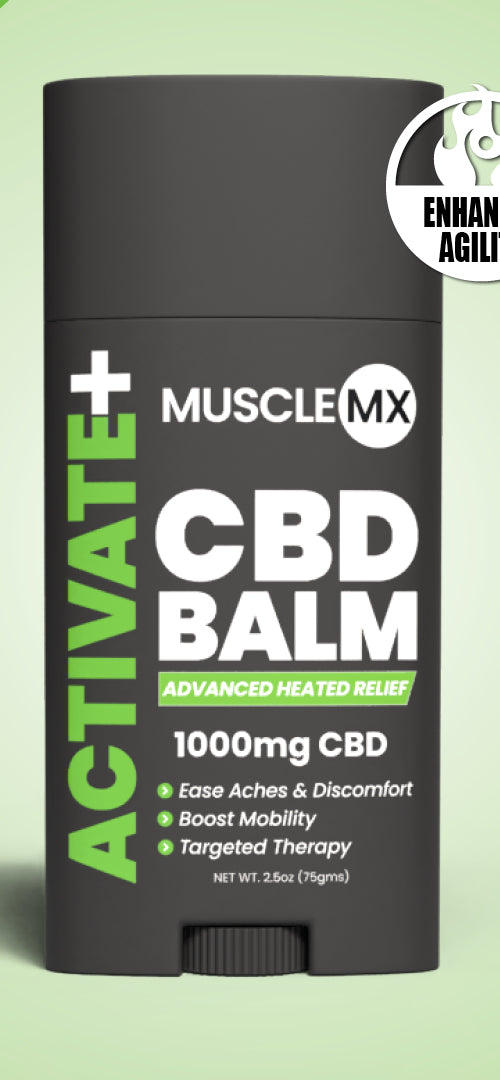
Pain treatment is a delicate art, and when approached with an evidence-based approach, it can be a powerful tool in improving one's quality of life. The key to effective pain management lies in understanding the various types of pain and the intensity of each individual's experience. At the heart of this approach are various techniques and treatments to manage pain, including non-opioid analgesics, nerve blocks, topical pain relievers, and interventional pain management techniques. These treatments can be tailored to each individual's specific needs and medical history, providing a comprehensive and practical approach to managing pain. Physical therapy and other forms of rehabilitation can also play a crucial role in pain management, helping individuals to improve their functional capacity and participate in daily activities. As discussed, keeping a pain journal or diary can be a valuable tool for tracking progress and adjusting treatment plans as needed. In severe pain cases, the use of opioids may be considered, but it is important to understand the limitations and potential risks associated with their use. Therefore, it is always best to work closely with a healthcare provider and pain management specialist to create a comprehensive treatment plan that addresses the root cause of the pain and strives for pain-free wellness.
The Takeaway
The art of pain management is intricately tied to the ability to articulate the nuances of one's pain to those who can help. By embracing the challenge of describing the various aspects of our pain, we become the narrators of our own health story, illuminating the complexities of our pain experience to those who can provide relief. Using descriptive words and creative phrasings, we can paint a vivid picture of our pain, including its unique sensations, intensity, and impact on our daily lives. Communication, whether verbal or written, is one of the most important tools in pain management and healing. At Muscle MX, we understand the importance of communication in the quest for a discomfort-optimized life. Communication is critical, and the right resources can help bridge the gap between you and your healthcare provider, empowering you to take a more active role in your well-being. Sources: Chronic Pain and the Health of Populations | SPH Numeric Pain Rating Scale | Physiopedia Visual Analogue Scale | Yale Assessment Module Training
|